
Fungal infection very often affects toes or nails. This disease affects adults and children. To avoid the pathology becoming chronic, you need to know the signs of foot fungus and what such a disease looks like.
The main signs of the disease
Of all skin diseases, mycosis of the feet is the most common. You can catch the disease by neglecting basic hygiene rules. Sometimes it is very difficult to cure the fungus.
For each person, foot fungus begins and develops in its own way. Here are the most common signs of foot fungus:
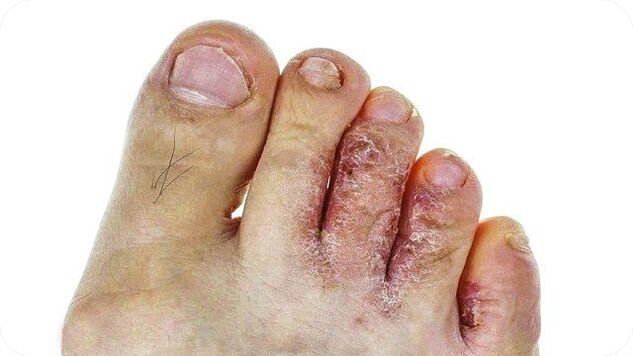
- characteristic cracks appear between the fingers;
- You can tell that the fungus has appeared by the characteristic itching on the feet and between the toes;
- the skin of the feet is very dry, often peels and becomes rough;
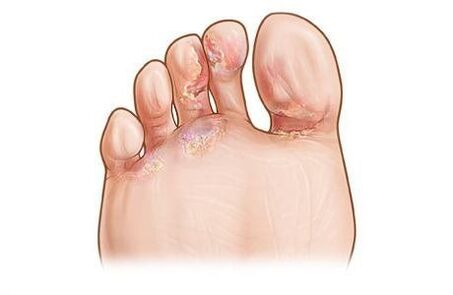
- blisters appear between the fingers, which burst when destroyed;
- the infection can spread to neighboring areas;
- reddish spots appear on the skin that cause significant discomfort;
- You can also recognize foot fungus by its unpleasant smell.
When the first symptoms of the disease appear, immediately consult a dermatologist. If you do not do this in advance, it will be much more difficult to treat the fungus.
Signs of fungus depending on the type of pathogen
This disease develops due to different types of pathogens. Symptoms of foot damage will vary in each case.
- If a yeast fungus develops on the feet, the nail gradually becomes thinner and peels off from the bed. The skin on the foot is hyperemic (takes on a red hue).
- With the development of epidermophytes, the nail turns yellow and becomes covered with spots. The skin of the feet peels off and emits an unpleasant smell. A characteristic symptom of this type of fungus is increased dryness of the skin.
- When mold fungus appears, the nail plate can suddenly change color. The skin becomes red if the pathogen gradually spreads to the entire foot. The person suffers from itching, and the skin may crack. In this case, pain and other unpleasant sensations appear while walking.
Only a doctor can determine the type of pathogen. This cannot be done at home. And if you engage in self-medication, you can only harm yourself. Your legs will suffer from it, and the fungus on the skin will spread more and more.

Signs of some forms of fungus
Depending on the affected area and the degree of development, several forms of pathology are distinguished. The symptoms of each of them are different. By knowing the early signs of foot disease, you can start treating mycosis in time.
- Interdigital dermatophytosis is the most common stage of the disease. It becomes more active in spring and summer, when the feet sweat the most. Cracks and sores appear between the fingers. You can notice the presence of scales on their skin. The foot looks absolutely healthy. Often a person feels itchy.
- The deleted form appears to the smallest extent. Peeling between the fingers is noticeable. At this stage of the disease, a sharp unpleasant smell spreads from the feet: it appears due to increased activity of bacteria.
The disease can appear in different forms. Let's get acquainted with their signs so that we know how to recognize foot fungus and, if it develops, start treatment. It must be remembered that in the advanced stages of the disease, the nail is completely destroyed. It is almost impossible to restore it.
Squamous type
This fungus is characterized by intensive peeling of the epidermis. Moreover, the areas of skin between the toes and the side of the foot are most intensely affected. There are no signs of an inflammatory process. In the photo of the first signs of foot fungus, areas of hyperemia are visible. Squamous fungus looks like this:
- the stratum corneum thickens;
- skin shines, sometimes becomes thick;
- the pattern on the skin becomes clearer;
- the fungus gradually spreads to the fingers, the entire foot and affects the nails;
- sometimes lamellar scales appear on the epidermis;
- The patient does not feel any other unpleasant sensations.
Dyshidrotic type
With this fungus, small blisters filled with liquid appear on the skin. They are usually located on the side of the foot. Then they gradually move towards the inner side of the fingers. How to recognize dyshidrotic foot fungus:
- the balloon is usually one, but if there are many, they merge into one big one;
- if left untreated, the fluid in the blisters gradually darkens;
- If the bubble bursts, an erosion with a crust appears in its place.
With this type of foot fungus, there is a very high risk of bacterial infection. The infection enters the body through open skin lesions.
Intertriginous type
This type of fungus is the most common. At first, the person does not feel any symptoms. Until a certain moment, the skin on the fingers does not change. After that, cracks and layers appear. The skin is not affected, but may sweat.
Candidiasis of the feet
The characteristic symptoms of this fungal infection are as follows:
- the lesion is the 3rd or 4th finger;
- the skin is red and swollen;
- There is a blister around the lesion where the peeled layer of skin is located;
- There are pustules and blisters nearby.
If a bacterial infection enters the affected area, it leads to an increase in local temperature. Swelling is noticeable on the skin of the legs. In severe cases, a person experiences general hyperthermia.
Signs of a fungal nail infection
One's toenails can also be affected. The disease can be distinguished by the following symptoms.
- Pronounced discoloration of the nail plate. Depending on the type of pathology the patient has, the nail takes on different shades. Sometimes it can change only on part of the nail plate.
- Nail crumbling. This happens only in advanced stages. If the nail is completely infected, it is destroyed.
- Changes in the structure of the nails.

There are several types of onychomycosis, a fungal nail infection.
- Atrophic appearance. The nail plate looks very thin. It darkens, sometimes takes on a grayish-brown color. The nail gradually peels off from the bed. The skin underneath becomes keratinized and becomes loose.
- In the normotrophic form of foot fungus, the plate changes color. Spots appear on it - white, yellow, green and even black. The structure of the nail is not affected.
- In the hypertrophic form, the plaque gradually thickens and becomes porous. The affected area looks very unsightly and in some cases causes pain when walking. It crumbles on the sides and collapses without treatment.
Some types of onychomycosis
Depending on the degree of spread of the disease, its forms differ.
- The most common is lateral onychomycosis. A small yellow spot first appears on the free edge of the nail. In the future, you will notice how it increases and the nail plate thickens. While walking, the person feels discomfort. The spreading of an unpleasant smell is noticeable. Lateral onychomycosis is difficult to treat.
- Superficial onychomycosis is characterized by damage to only the upper layers of the plate. It doesn't thicken, but becomes chalky over time.
- The rarest form of the disease is subungual onychomycosis. The skin thickens noticeably in the fold of the nail. The nail turns white and loses its transparency.
General principles of treatment
Any pathology treatment begins with a diagnosis. Only then can the appropriate medicine be prescribed. Self-medication usually leads to worsening of the condition of the legs. Let's get acquainted with the most common methods of therapy.
- At the first signs of a fungal infection, special varnishes, plasters, ointments and sprays are used. They must be used for a long time and according to the instructions.
- If local therapy is ineffective, complex antifungal drugs are prescribed. They are used orally.
- Surgical removal of the affected nail.
- Laser therapy.
- In advanced forms of the disease, systemic drugs are prescribed.
You can avoid the appearance of an unpleasant disease by following hygiene rules. Avoid using other people's personal hygiene products (towels, slippers). When the first signs of the disease appear, consult a doctor immediately.
Types of mycosis
Fungal infections of the feet usually occur between the toes. It is caused by several types of fungi. This problem is mostly characteristic of adults, because children's sweat can disarm the fungus.
Mycotic lesions can be of different types:
- candidiasis - occurs when the body's resistance decreases, most often in women;
- epidermophytosis is an exclusively "male" disease that develops due to excessive sweating;
- Rubromycosis is a highly contagious form that can occur even in young children.
Signs and forms of the disease
Signs of a fungal infection can vary depending on the age of the patient, the state of the immune system and the nature of the blood circulation.
In people with a strong immune system, the fungus can remain on the skin for several months without appearing. Slight itching and slight redness of the skin may occur.
Treatment and the best medicines

Advanced mycosis is treated with fungicidal tablets and antimycotic ointments. The latter are used after washing and drying the feet.
Folk remedies are recommended only in the initial stage of the disease, as well as to relieve itching. They must be used with great care as some rely on cauterizing the skin and can cause burns.
As for traditional medicine, they are used at the patient's own risk. Be especially careful when using formulations containing vinegar, celandine or manganese, as this can cause skin burns.
In parallel with drug treatment, you can use baths with oak bark, chamomile or sage. A soda bath effectively reduces itching.
Preventive measures
Although there are effective and inexpensive treatments for toenail fungus on the market, it is best not to allow the problem to develop. Prevention of fungal infection consists of:
- in daily hygiene;
- wearing individual footwear (especially in public showers, bathrooms and swimming pools);
- regular treatment of the inside of shoes with ammonia;
- daily change of socks;
- strengthening and maintaining immunity.
These are basic, simple measures that anyone can do. But if an infection occurs, then in order to prevent recurrence, it is necessary to treat foot fungus with drugs for another 14 days after the complete disappearance of all mycosis symptoms.
Fungus on the feet: symptoms and treatment, photo of fungus on the feet

Foot fungus is one of the most common diseases in dermatological practice. It occurs primarily in cultures where it is customary to wear shoes most of the time and affects up to 70% of the adult population.
Most often, foot fungus is observed in the elderly, as well as in those whose immunity is significantly weakened, for example, in diabetes, AIDS, circulatory disorders of the lower extremities and other diseases of this type.
Often, the term "fungus or mycosis of the feet" refers to damage by mycelium of fungi on the plantar skin of the feet, nails and interdigital spaces.
Pathogens
Among the many types of fungi, the main causes of foot mycosis are the following:

- Trichophyton rubrum,
- Trichophyton mentagrophytes,
- Epidermophyton floccosum.
Other causes of fungal foot infections, which are not so common:
- Trichophyton tonsurans is the causative agent of mycosis in children in America,
- candida,
- Scythalidium hyalinum,
- Scythalidium dimidiatum.
All the causative agents of fungal infections have adapted to parasitize in the stratum corneum of the skin, producing special enzymes that break down keratin. In addition, their membranes (cell walls) contain mannan - special substances that suppress local immunity and contribute to the development of chronic inflammation.
Routes of infection and factors contributing to the onset of the disease
It is believed that some types of fungal foot pathogens are able to maintain their viability in the scaly scales of the skin for a year. In order to become infected with the fungus, it is enough for such skin flakes with the pathogen to stick to the legs, and then fall into conditions suitable for reproduction: humidity and heat.
The most common foot fungus infections occur:
- In public places: baths, beach beds, swimming pools, saunas, even just sand on the beach.
- In the family: common household shoes, lack of individual towels for the feet, low level of hygiene.
- Habits: exchanging shoes, socks, wearing other people's shoes (for example, the house slippers of the visiting host).
Factors contributing to infection:
- Reduction of local protective forces as a result of circulatory disorders (for example, with vasculitis, obliterating atherosclerosis of the lower extremities), certain chronic diseases (HIV, other immunodeficiency conditions, diabetes mellitus, etc. ).
- Prolonged sweating of the feet in athletes during long training sessions, in the summer when they wear closed or poorly ventilated shoes.
- Cracks and macerations on the skin of the feet.
In general, men get sick more often than women, the frequency of fungal foot infections increases with age. The risk group for fungal foot infections are:
- miners,
- military personnel,
- customers,
- regular baths and saunas,
- athletes.
Types of diseases
According to the location of the pathological focus of the skin on the foot affected by fungi:
- Interdigital mycosis (dermatophytosis). It is most often observed in the form of chronic (squamous) or acute (intertriginous) forms.
- Plantar mycosis. It is most often manifested as peeling and keratinization of the skin of the feet.
- Dyshidrotic dermatophytosis. Bubbles and vesicles form on the skin of the feet, which often resemble allergic dermatitis.
- Deep mycosis. In this case, not only the superficial but also the deep layers of the skin are affected.
- Onychomycosis. Fungal nail infection.
Depending on the type of pathogen, the main fungal diseases of the feet are:
- Athlete's disease caused by Trichophyton mcntagrophytes.
- Rubrophytosis caused by Trichophyton rubrum.
Rubrophytosis of the feet: main types and symptoms
Rubrophytosis is the most common fungal disease of the feet. It occurs in almost 70-90% of cases.
Symptoms
The classic form of rubrophytosis is characterized by redness and moderate thickening (lichenification) of the skin. The affected skin is shiny, with an increased pattern, dry surface with mealy scales accumulated in the area of grooves and folds.
Usually the disease begins with the third or fourth interdigital folds, which are the most severe. The fungus then spreads to other spaces between the toes, the plantar part and the back of the foot.
The following forms are characteristic of rubrophytia:
Often encountered:
- squamous form (the main symptom is peeling skin),
- keratinizing form - the presence of "corns", thickening.
- intertriginous (opreloid),
- dyshidrotic (with blistering),
- mixed form (diaper rash, blisters).
On the leg
Eradicated squamous rubrophytia has the least pronounced symptoms and goes almost unnoticed by the patient. Its main symptoms:
- Interdigital spaces: peeling, presence of mealy scales, surface small cracks.
- There are practically no complaints or you may be bothered by minor itching.
In this form, rubrophytosis can last quite a long time. However, the progression of the disease is gradually observed, which leads to the appearance of hyperkeratotic and mixed forms. They appear gradually:

- increased dryness of the skin of the feet,
- skin roughness,
- the appearance of rough blisters on the soles and sides of the feet,
- formation of deep and painful cracks in the heel area.
With rubrophytosis of the feet, 3 main types of skin peeling are observed:
Flourous. The natural folds and furrows of the skin seem to be sprinkled with flour.Ring-shaped . Reddish spots with a rim of exfoliated epithelium.Large-lamellar . In this case, the skin peels off in large slabs.
In interdigital spaces
During intense sweating of the feet, wearing shoes with poor ventilation or inadequate treatment, the spaces between the toes occasionally start to get wet. The skin becomes swollen, eroded, with deep cracks. The main complaints of patients at this stage are itching, pain, burning.
Without timely and effective treatment, the process gradually worsens, which is manifested by increased pain and itching, which are intensified by movement. On the skin of the interdigital spaces and the lateral surfaces of the fingers, large blisters appear, which then turn into erosions, surrounded by a rim of whitish epidermis.
On the nails
Nail plates of the toes with rubrophytosis:
- condensed,
- decomposition,
- yellowish-gray or with a brown tint,
- sculpted white spots that later spread to the entire nail.
Sometimes they separate from the nail bed, thicken and take on the appearance of a bird's claw or an ingrown nail, which causes additional discomfort to patients.
Complications of rubrophytosis
As a rule, rubrophytia spreads to other parts of the body: hands, smooth skin, hair. The pathogen enters new areas of the skin by lymphogeny, as well as by contact (for example, it is transmitted by hands when washing the feet).
- Hands - damage to palms and nails.
- Smooth skin - lesions on the face, inguinal-femoral folds, buttocks, legs.
In this case, mycosis manifests itself as round pink-red or pink spots with a tendency to coalesce and peripheral growth. Their surface is covered with scales, and along the edges there is an inflammatory ridge with small bubbles and crusts.
If rubrophytia has spread to large folds, itching occurs.
Athlete's foot: types and symptoms
Athlete's foot occurs much less often than rubrophytosis and has the same forms of the disease:
- Deleted.
- keratinization.
- Diaper rash.
- With the formation of bubbles.
- Athlete's nails.
Then, plaque-like thickenings of bluish-red skin appear on the lateral surfaces and soles. In the center of the rash there are layers of scales, the boundaries of the lesions are clear. In the spaces between the fingers, the epidermis acquires a whitish hue.
With athlete's foot, patients suffer from itching, increased dryness and pain on the skin.
Opreloid (intertriginous) form of epidermophytosis is characterized by redness, swelling and maceration of interdigital folds. Cracks often form and pain is felt.
When the pathogen infects the arch of the foot, a dyshidrotic form can often be observed with the formation of blisters, which after opening look like pink or red moist erosions.
Athlete's foot most often occurs on the big toe (I) and little toe (V). In the thickness of the nail, closer to the free edge, yellowish spots and stripes are formed, which gradually increase in size and occupy the entire nail. Then, the nail begins to crumble, sometimes peeling from the nail.
Acute epidermophytosis Podvysotskaya
The main symptoms of this form of athlete's foot:
- swelling of feet, toes,
- abundance of vesicles,
- weeping erosions,
- maceration of interdigital folds,
- enlarged inguinal lymph nodes,
- increase in body temperature,
- headache,
- difficulty walking due to pain,
- general weakness.
Onychomycosis of the toes: symptoms and types
In addition to the causative agents of rubrophytosis and epidermophytosis, onychomycosis can be caused by yeast fungi of the Candida genus, as well as some other fungi.

The most typical symptoms of onychomycosis, which begin closer to the free edge of the nail:
- discoloration, loss of natural shine,
- thickening of the nail plate,
- occurrence of subungual hyperkeratosis,
- destruction of the nail, separation from the nail bed.
In onychomycosis, there are 2 main types of nail damage:
- Normotrophic: stripes of white and yellowish color are visible in the thickness of the nail.
- Atrophic: thinning, destruction of the nail plate, its separation.
Diagnosis of fungal foot infections
A specialist in the treatment of fungal infections of the feet is a dermatologist who, if necessary, can include other specialists in the treatment.
After talking with the patient, clarifying the complaints and characteristics of the onset and course of the disease, the doctor will examine the affected area and prescribe some types of additional examinations, for example:
- Microscopic examination with additional treatment of the material with potassium hydroxide.
- Wood's lamp test.
- Inoculation of suspected biological material on special media for the growth of fungi, as well as on media for bacteria.
Treatment
Treatment for any fungal foot infection must be prescribed by a doctor in order to achieve a complete cure.
In general, the treatment of foot mycoses is based on the following principles of therapy:
- The fight against the infectious agent. In the initial stages of the disease, local drugs are usually prescribed - antifungal ointments, creams, lotions. In severe cases, use systemic antifungal drugs.
- Increasing immunity and improving local blood circulation, treatment of the underlying disease.
- Desensitizing therapy. Since foot mycosis is often accompanied by allergic reactions, anti-allergic drugs are prescribed accordingly, which will help improve the patient's condition.
Treatment at home
- For the effective treatment of mycosis of the feet, it is necessary to remember that fungi multiply in a moist environment. By excluding moisture, fungus will not develop and the chances of healing will increase.
- Protect your family members from fungal diseases. Explain to them that from now on you can't walk around the apartment barefoot, especially in the bathroom or shower. After bathing or showering, it is necessary to treat the bathtub itself, the tray and the floor with disinfectant.
- Wash your feet with soap every day, collecting all the loose pieces of skin with a towel so that nothing gets under the nails.
- After washing your feet, be sure to dry the spaces between the toes with toilet paper or a hair dryer, and then apply an anti-fungal agent prescribed by your doctor. Treatment must be continued for several months even in cases where the manifestations of mycosis completely disappear.
- Use powder while wearing shoes.
- Wear white cotton socks (clean every day). Used socks should be boiled or soaked in disinfectant for 10 minutes. Shoes must be disinfected with antifungal sprays.
Prevention of foot mycosis
Timely treatment of diseases that can reduce the body's defenses or impair blood circulation.
Conclusion
Fungus on the feet is one of the most common fungal skin infections. In most cases, following simple rules of prevention helps to avoid the disease, and timely treatment begins to completely get rid of mycosis.

























